The burden of healthcare costs varies across age, sex, location, and socioeconomic status, but the elderly, women, rural, and poorer Filipinos are more likely to pay out-of-pocket healthcare costs, according to a study of state think tank Philippine Institute for Development Studies (PIDS).
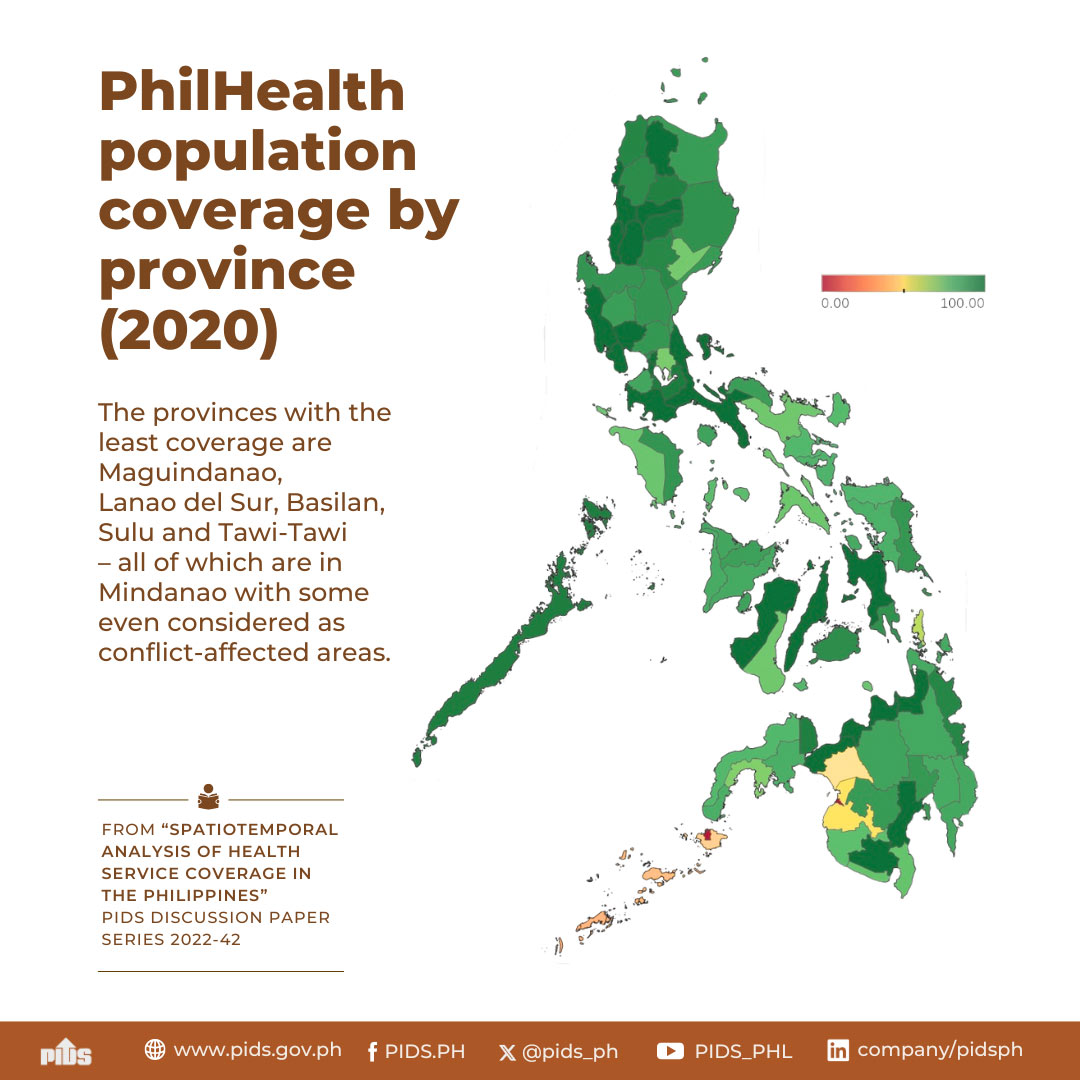
In “Spatiotemporal Analysis of Health Service Coverage in the Philippines”, authors PIDS Senior Research Fellow Valerie Gilbert Ulep, Supervising Research Specialist Jhanna Uy, and research consultants Clarisa Joy Flaminiano, Vicente Alberto Puyat, and Victor Andrew Antonio examined the financial risk protection of Philippine Health Insurance Corporation (PhilHealth) members and dependents. It computed the “support value” or the percentage of hospital care cost shouldered by PhilHealth using 2018-2021 PhilHealth data along with auxiliary datasets from the Department of Health (DOH), Philippine Statistics Authority, and Washington-based Institute for Health Metrics and Evaluation.
Ulep and co-authors observed that PhilHealth members still pay out-of-pocket because the National Health Insurance Program covers only 40 percent or lower hospital costs.
Out-of-pocket health costs remain a significant expense among households and are “expected to increase for the entire population” in the coming years.
“Effective financial protection in a health system should reduce out-of-pocket patient costs that are not covered by insurance as much as possible,” they said.
The average support value is 55.83 percent in the Philippines. Still, the percentage varies based on PhilHealth membership type, socioeconomic status, patient accommodation, disease classification, hospital ownership and level, and location.
For instance, the study found that indirect contributors have lower support value than direct contributors on average, but at-risk subpopulations enjoy “more consistent coverage” due to existing benefits offered to indigents and sponsored beneficiaries.
Elderly members, who have less income yet incur the biggest health expenses, got the lowest support value in public and private hospitals.
Women face higher financial risk due to lower income and higher hospital admission rates across all age brackets for “avoidable conditions” that could have been addressed through outpatient and preventive care. The authors said the high admission rates suggest an “ineffective and inefficient” primary healthcare system, making health care “more expensive” for patients and the health system.
People in provinces where most PhilHealth members are indirect contributors possess higher financial risk because they have less income for health care.
The study added that Filipinos in rural areas are likely to spend more because of the “maldistribution” of primary care facilities and accredited hospitals that “do not cover the cost of all services”. Only 43 percent of Level 1 hospitals, which offer minimum healthcare services, are government-owned.
“Some benefit packages are only available in government-owned hospitals. PhilHealth should endeavor to develop benefit packages responsive to the health needs of different subpopulations and available across hospital levels and ownership,” the authors said.
Ulep and co-authors highlighted that members seeking care in private rooms and in private and Level 3 hospitals (with below 45% support value) also face “higher financial risk”. They added that private accommodation for intensive cases and care in wards must become affordable because they allow for “better environment and better outcomes” for maternal, neonatal, and similar types of care.
The study reported that 14 of the top 15 diseases with the highest claims from 2018 to 2021 received varying support value even if the conditions have similar health risks. All received below 50 percent support value.
To address the “financial risks of catastrophic health expenses”, the authors recommended a “strategic shift” in PhilHealth’s service purchasing and revenue generation to guarantee sufficient funds for all covered diseases.
They advocated shifting from case-based to diagnosis-related groups-based system to address the varying range of support value across related diseases. They also recommended providing essential services outside of hospitals, investing in health literacy, and increasing the support value for elderly beneficiaries.
This press release is based on the PIDS discussion paper titled “Spatiotemporal Analysis of Health Service Coverage in the Philippines”. ###